The itchy cat
We’re all familiar with people who are allergic to cats. But cats can be allergic to stuff too (no, they don’t seem to be allergic to people). And when they are, they get itchy – this is called feline allergic skin disease.
What is feline allergic skin disease?
Feline allergic skin disease (FASD) is just that – skin disease due to allergy.
Allergy
An allergy is an altered (exaggerated) immune response to a normally harmless substance (called an allergen). There are endless potential allergens but cats are generally affected by three main types of allergies:
flea allergy
food allergy
environmental allergy (called atopy and includes things like pollens, moulds, dust mites)
The exaggerated immune response to these allergens is itchiness (pruritis) and the itchiness occurs in particular places with specific appearances. As the cat scratches (or overgrooms) these itchy places we see fur and skin changes called cutaneous reaction patterns.
Here's a quick look at the four different reaction patterns.
Papulocrustous (miliary) dermatitis
feels bumpy
lots of tiny scabs
hair loss due to licking hard and breaking the hair shaft
often noticeable over the rump (but can be anywhere)
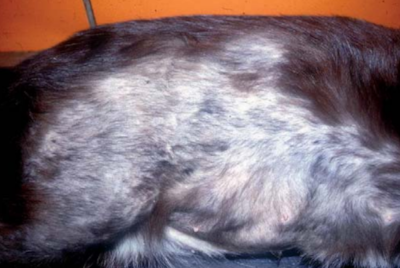
Symmetrical self-induced alopecia
areas of baldness that appear symmetrical
often on the belly and inner thighs
can involve the trunk, bum and backs of thighs
may have some sores where the tongue has abraded the skin surface
Eosinophilic lesions
Different appearances:
erosions/ulcers on the lips
nodules and/or plaques on the body (usually belly or thighs) – these may have a linear appearance
As awful as these look, they can respond well to treatment
Head and neck excoriations
hair loss and skin breakages due to scratching
range from mild to extreme
often the hardest of all to treat
The pattern of skin disease is very useful for predicting the type of allergy in dogs. But, when it comes to cats, the reaction patterns are not specific for any particular allergen.
Flare factors
Along with the allergens themselves, allergic cats can get itchy because of 'flare factors'. These are other things that exacerbate the itch and include:
secondary bacterial infections
secondary yeast/fungal infections
fleas (for animals without a flea allergy, fleas can be a flare factor)
psychogenic factors (eg stress)
dry skin
If these things are present, they need to be treated in addition to the allergy.
The itch (pruritic) threshold
An important concept to be aware of with FASD is the itch threshold. It's also called the pruritic threshold or the clinical threshold, and it's the point when your cat begins to experience severe itching due to a summation of 'events' (ie exposure to allergens and also flare factors). The pruritic thresholds are unique in each animal. Thresholds can also go up and down with things like stress and anxiety.
Here are some examples.
Example 1. A cat has a threshold of 40 'itch units'
She has a flea allergy that contributes 45 itch units so fleas alone will cause severe scratching/overgrooming
Good flea treatment should control her symptoms
Example 2. A cat has a threshold of 60 itch units
She has a mild flea allery (contributes 45 itch units) so can tolerate some fleas without severe scratching/overgrooming
But if she develops a secondary infection, her threshold is reached and she starts scratching/overgrooming
If we remove the fleas or treat the secondary infection, the itch units will return to below the threshold and the scratching/overgrooming will resolve
Example 3. A cat has a threshold of 50 itch units
She has a mild flea allergy (contributes 35 itch units)
She has a mild mould allergy (contributes 25 units)
If she develops a dry skin condition this will contribute 20 units
None of these alone will cause her to scratch/overgroom severely, but if they occur in combination, her threshold might be reached and she'll start to scratch
The summation effect explains why a cat who is mildly allergic to one or two allergens (eg mould, pollens) can appear to be completely normal, until she develops a new allergy (eg to fleas) or skin condition.
The primary allergies
Flea allergy
A flea allergy is more specifically an allergy to a protein in flea saliva. So your cat needs to be bitten by a flea to trigger the allergy (it won't happen by fleas just crawling around). Unfortunately, when a flea jumps on, it will bite and feed within about 3–5 minutes.
By the time you see the signs of allergy, the flea/s that triggered it may be long gone – groomed away and swallowed by your cat.
DISTRIBUTION OF SKIN LESIONS
Areas of the skin most likely to be itchy due to flea allergy include: rump, backs of thighs, belly and head.
REACTION PATTERN
Flea allergy can cause any of the four reaction patterns. Flea allergy is responsible for:
35% of papulocrustous dermatitis
39% of symmetrical alopecia
38% of head and neck excoriations
14% of eosinophilic granuloma lesions
DIAGNOSIS
We can't rule out flea allergy just by not seeing fleas or flea dirt – in fact, about 50% of cases diagnosed with flea allergy in the specialist setting will have never had visible fleas. Cats are just incredibly fastidious groomers.
Also, using flea control doesn't exclude flea allergy. Most products don't kill fleas quickly enough to prevent them biting/feeding... and fleas can become tolerant to products as well.
Diagnosing a flea allergy involves doing a therapeutic trial with a product that is known to kill fleas quickly and that fleas haven't become resistant to. The product currently recommended is Bravecto® spot-on. After application, we assess itchiness/skin lesions over 30 days:
a good response (ie >80% improvement) means your cat is very likely to have flea allergy
a moderate response (ie 30–80% improvement) means we continue the trial for another month (no further application of Bravecto is needed as it lasts for 3 months, we just keep monitoring
if there is not further response with the additional time, it's likely that your cat has FAD but also has a concurrent allergy (food allergy or atopy)
a poor response (ie <30% improvement) means your cat is unlikely to have flea allergy
TREATMENT
There is no cure for flea allergy. If flea allergy is confirmed, year-round flea control is needed to reduce exposure to flea saliva.
Food allergy
The most common allergens in food are beef, fish, chicken and dairy. A food allergy can develop at any age, but most cats start to show symptoms before 3 years of age. It's important to realise that food allergy develops over time. It doesn't occur with a change of diet. It might not cause any gastrointestinal signs either.
Both male and female cats are equally affected by food allergies. However, some breeds may be at increased risk (eg Birman, Abyssinian and Siamese).
DISTRIBUTION OF SKIN LESIONS
Areas of the body most likely to be itchy due to food allergy include: head and face, neck and belly.
REACTION PATTERNS
Food allergy can cause all of the four reaction patterns. That said, head and neck excoriations are more frequent than papulocrustous dermatitis with food allergy.
DIAGNOSIS
The only way to diagnose a food allergy is by feeding an elimination diet, seeing a resolution of signs and then seeing a relapse with the reintroduction with previously fed foods. Blood tests and intradermal tests are unreliable for diagnosing food allergy in cats.
The food most commonly recommended by dermatologists for a food trial is Royal Canin® Anallergenic. For cats that don't like a total dry food diet, a novel protein source can be added (eg goat, crocodile).
You need to feed the trial diet for 6–8 weeks and then assess the response:
80% of cats with food allergy show improvement at 6 weeks
90% of cats with food allergy show improvement at 8 weeks
You can then add back a single protein at a time to see what causes the symptoms to return.
TREATMENT
There is no cure for food allergy. Treatment involves avoiding the foods your cat is allergic to.
Lots of people chose not to do the 'challenge to relapse' part of the trial and just stick to the hypoallergenic diet long term as the treatment. This is fine if a balanced diet like Anallergic is used. But if you're doing a home prepared elimination diet, you'll need help in turning it into a long term diet (see BalanceIT).
Environmental allergy (atopy)
Unless we do allergy testing, we can't really say what your cat is allergic to in the environment. But common causes are:
pollens (from grasses, weeds and trees)
moulds
dust mites and storage mites
skin cells of other animals (dander)
Pollen allergies are very common. If your cat gets itchy (or has worse itch) during certain times of the year, she might have a pollen allergy because these are usually seasonal. For example:
grasses (eg ryegrass) start pollinating (releasing pollen) in late spring and go through to late summer
weeds (eg ragweed) usually pollinate late summer
trees (eg plane trees) pollenate early spring
The Australia Society of Clinical Immunology and Allergy have a nice pollen calendar if you want to know when common allergenic plants are going gangbusters.
While moulds can cause allergies all year round, there are often spikes during spring and autumn. We may see thresholds being reached during these times.
There is no known age, sex or breed predilection for atopy in cats like we se in dogs and people. This may change as more research is done.
DISTRIBUTION OF LESIONS
Areas of the body most likely to be itchy due to atopy are the head and belly. But as with all feline allergies, we can see fur and hair changes anywhere on the body.
REACTION PATTERN
Atopy can cause all of the four reaction patterns. There is no way to tell the difference between food allergy and atopy based on the reaction pattern.
DIAGNOSIS
We reach a diagnosis of atopy by excluding other causes of itch. That is, if we've seen no response to a flea therapeutic trial or elimination diet and there is no secondary infection, then we come to the clinical diagnosis of feline atopic dermatitis.
Blood testing (serology) and intradermal testing aren't used to diagnose atopy. They're used to determine what specific things your cat is allergic to.
TREATMENT
Atopy is not curable. As with all the allergies, treatment aims to control itching and improve quality of life. There are several treatment options, but none of them will make your cat itch-free forever.
Treatment options include:
Antihistamines – it's rare for us to find that antihistamines control itch really well. That said, because they are so safe and well tolerated, they're worth a try. And if you find that 1/4 of a Zyrtec® or Claratyne® helps, great! Keep going!
Corticosteroids – these usually work very well. There are some experts who say that they're less effective in food allergy than in other allergies. Cats are relatively resistant to the side effects of cortisone based medications, which is just as well as they require relatively larger doses than dogs. Corticosteroids are available in oral formulations (tablet and liquid) and injectable formulations
Cyclosporin – this can be very effective but has downsides of taste, expense and side effects (gastrointestinal signs and a fleshy overgrowth of the gums called gingival hyperplasia)
Immunotherapy ('allergy shots') – an individual formulation is made for each patient based on allergy testing (serology or intradermal testing). The formulation is injected in increasing doses to desensitise the immune system to the allergen. While it's a pretty involved and expensive process, over the long term it can work out to more effective (in controlling symptoms and in terms of cost) than other treatments. Immunotherapy is also safe and has no negative effects on the immune system.
The 'newer' treatments for dogs Apoquel® and Cytopoint® are not useful in cats.
The flare factors
Psychogenic factors
Some cats will overgroom due to stress. They can make themselves remarkably bald without you actually seeing them licking excessively. They often do it in secret.
It's possible to have allergic skin disease and stress overgrooming at the same time. We might find that treating the allergy brings the itch below the threshold but in some cases, we might also need to address the stress.
Bacterial infections
Sometimes it's pretty obvious that we're dealing with a secondary bacterial infection (eg smelly pus is present). Other times, we might need to go looking by taking samples from the skin and looking at them under the microscope.
Secondary infections usually require oral or injectable antibiotics as topical therapies are rarely highly effective.
Yeast/fungal infections
Secondary infection with a yeast/fungus called Malassezia is not uncommon. These microbes live naturally all over the skin but will rapidly overgrow and cause trouble if the conditions of the skin change. The change they most like is increase in moisture (eg from saliva or moist dermatitis).
Malassezia can give off a stink but we usually confirm overgrowth by taking a sample from the skin and looking at it under the microscope.
Topical and oral therapies are available.
Dry skin
This can occur with change of seasons and shedding, poor diet and lack of grooming (eg old age, dental disease, arthritis).